Knee arthritis
Mr Khitish MohantyConsultant Trauma & Orthopaedic Surgeon, UK
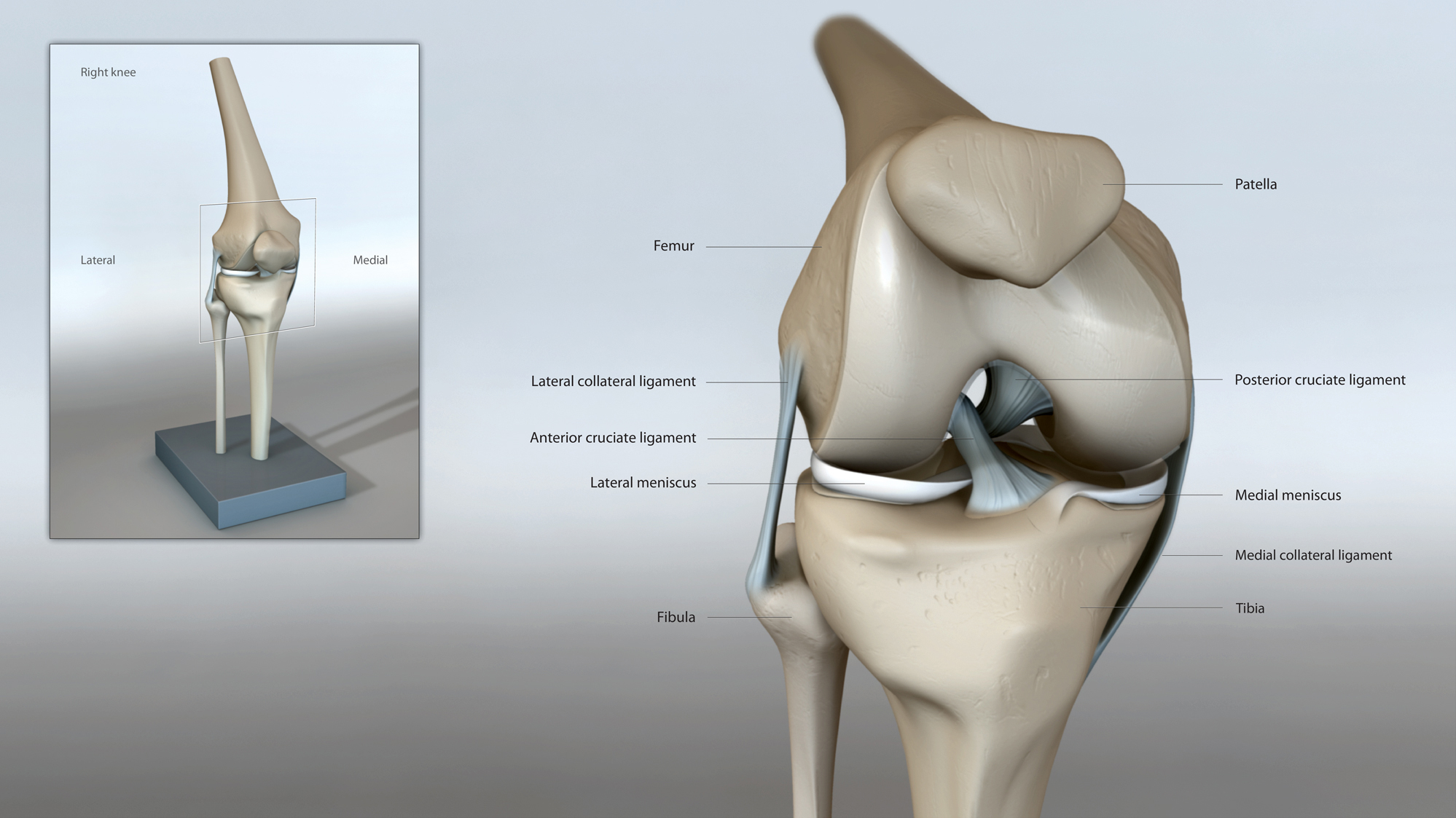
Knee Joint
The knee joint is the joint between the femur (thigh bone) and tibia (leg bone) and also the patella (kneecap). The surface of these bones are covered with special cartilage called the articular cartilage. The smooth surface of the articular cartilage along with the natural lubrication allows smooth gliding movement of the joint surface.
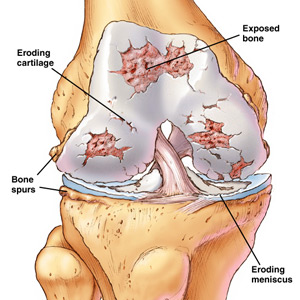
Arthritis of the Knee
Knee arthritis is very common and mainly results from wear and tear called osteoarthritis or degeneration. The knee joint can also be affected by inflammatory arthritis such as rheumatoid arthritis and gout etc.
Symptoms and Signs
Patients complain of pain particularly on weight bearing and walking. They also find the knee to be swollen and visible deformity develops in the later stages. The patient’s knee becomes stiff and they struggle to walk, climb stairs and carry out other activities of daily living.
Assessment
After a careful history, the knee is clinically examined. In most cases a plain x-ray of the knee particularly on weight bearing position provides the appropriate diagnosis. In some cases, particularly when patients have mechanical symptoms such as locking, jamming, catching and giving way an MRI scan may be helpful.

About Knee Replacement
MANAGEMENT
Initial management is non operative or conservative. This includes the use of painkillers, anti-inflammatories, physiotherapy and activity modification. In cases which do not respond to medication, an intra articular steroid injection has shown to provide temporary benefit. In patients with moderate arthritis who are relatively young but have mechanical symptoms such as locking or giving way, keyhole surgery is considered where the knee joint is cleaned out.
KNEE REPLACMEMENT
When the arthritis is too advanced or patients do not respond to non operative treatment, a partial or a total knee replacement is considered. In total knee replacement the surgeon resurfaces the knee joint with an artificial knee with metal and plastic component. In the majority of cases the knee replacement is fixed to the patients bone with bone cement. In selective cases where only one compartment of the knee is involved and the rest of the knee has been found to be entirely normal, a partial knee replacement could be carried out. This operation is less morbid and is done through a smaller incision resulting in a quicker recovery.
POST-OPERATIVE
Most patients, after a knee replacement, are mobilised either on the day of the operation or the day after. The leave hospital after two to three nights stay. They are asked to use crutches for approximately four to six weeks. Post-operative physiotherapy is incorporated in the management.
OUTCOME
A total knee replacement is still one of the most successful operations. The majority of patients experience pain relief and good functional outcome. However, a proportion of patients may still have moderate residual discomfort despite a technically successful knee replacement. Activities like kneeling, squatting etc may be limited after a knee replacement.
RISKS AND COMPLICATIONS
Complications such as infection, stiffness, wound healing problems; deep vein thrombosis and pulmonary embolism etc are uncommon but are seen occasionally after knee replacement. Appropriate prophylaxis is carried out to prevent known complications such as infection and vein thrombosis.
